Preeclampsia: Understanding This Serious Pregnancy Complication
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and signs of damage to other organ systems, most often the liver and kidneys. It usually begins after 20 weeks of pregnancy in women whose blood pressure had previously been normal. Left untreated, preeclampsia can lead to serious, even fatal, complications for both the mother and baby. Recognizing the signs and symptoms, understanding the risk factors, and knowing the treatment options are crucial for managing this condition.
1. What is Preeclampsia?
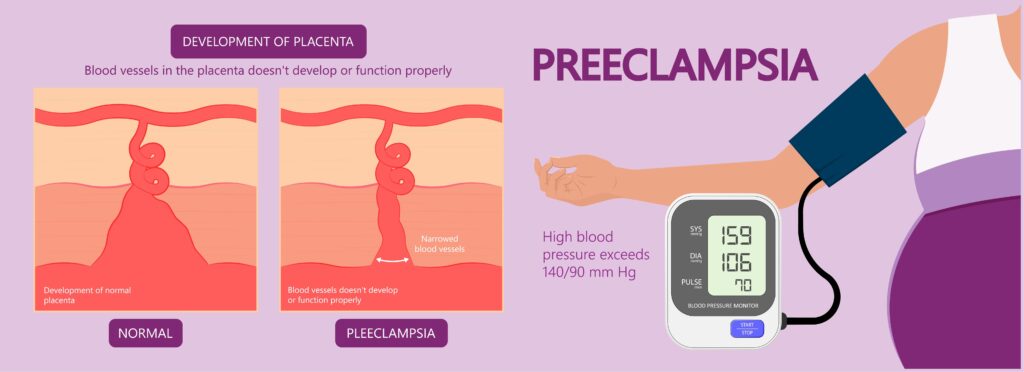
Preeclampsia is a hypertensive disorder that occurs during pregnancy. It affects approximately 5-8% of pregnancies and is one of the leading causes of maternal and fetal morbidity and mortality worldwide. The exact cause of preeclampsia remains unknown, but it is believed to result from abnormal development of the placenta, leading to poor blood flow and an immune response that affects blood vessel function.
2. Symptoms of Preeclampsia
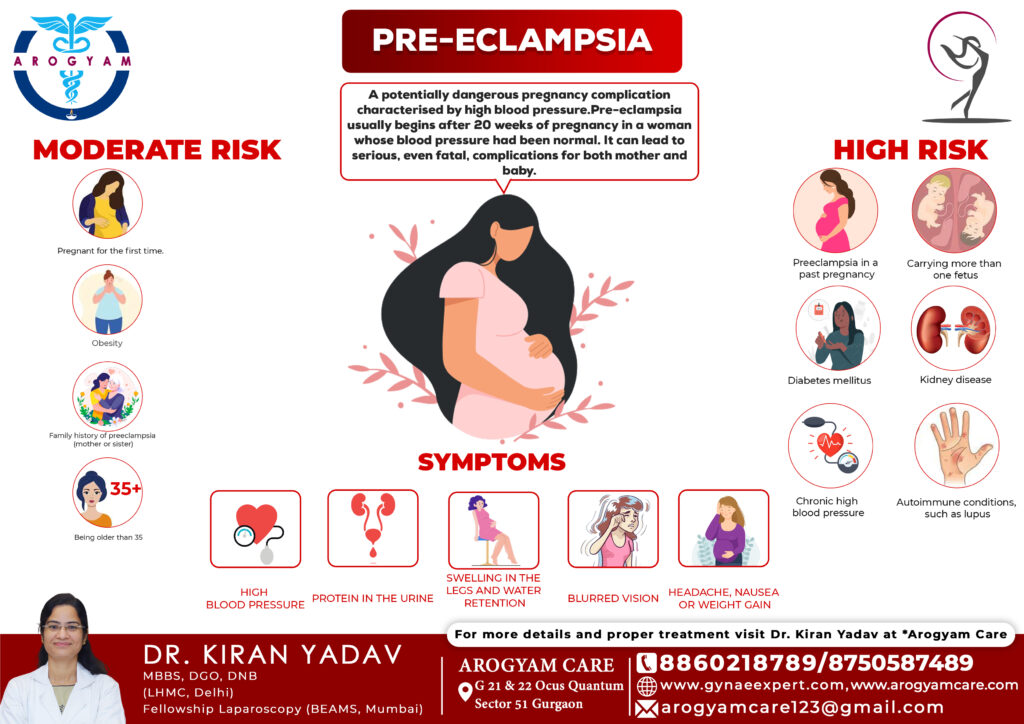
The symptoms of preeclampsia can vary, and some women may not experience any noticeable symptoms. However, common signs and symptoms include:
-
High Blood Pressure: A key sign of preeclampsia is a sudden increase in blood pressure, typically above 140/90 mm Hg. Blood pressure readings are closely monitored during prenatal visits to detect any abnormalities early.
-
Proteinuria: The presence of excess protein in the urine (proteinuria) is a significant indicator of preeclampsia. Proteinuria is detected through routine urine tests during prenatal check-ups.
-
Swelling (Edema): Sudden swelling of the hands, feet, face, and legs can occur due to fluid retention. While mild swelling is common during pregnancy, severe or sudden swelling may indicate preeclampsia.
-
Severe Headaches: Persistent, severe headaches that do not go away with usual pain relief measures can be a symptom of preeclampsia.
-
Changes in Vision: Blurred vision, temporary loss of vision, light sensitivity, or seeing spots or flashing lights are concerning signs.
-
Upper Abdominal Pain: Pain under the ribs, particularly on the right side, may indicate liver involvement, a serious aspect of preeclampsia.
-
Nausea or Vomiting: Nausea and vomiting, especially after mid-pregnancy, can be symptoms of preeclampsia.
-
Decreased Urine Output: A decrease in urine production may occur as the kidneys are affected by the condition.
-
Shortness of Breath: This can be caused by fluid buildup in the lungs due to preeclampsia.
3. Risk Factors for Preeclampsia
Several factors can increase the risk of developing preeclampsia during pregnancy. These include:
-
First Pregnancy: Women experiencing their first pregnancy are at higher risk of developing preeclampsia.
-
History of Preeclampsia: Women who have had preeclampsia in a previous pregnancy are at an increased risk of recurrence.
-
Family History: A family history of preeclampsia, such as a mother or sister having the condition, raises the risk.
-
Chronic Hypertension: Women with pre-existing high blood pressure have a higher chance of developing preeclampsia.
-
Multiple Pregnancies: Women carrying twins, triplets, or more are at greater risk.
-
Maternal Age: Women younger than 20 or older than 35 are at higher risk.
-
Obesity: Obesity increases the risk of preeclampsia and other pregnancy complications.
-
Certain Health Conditions: Conditions such as diabetes, kidney disease, autoimmune disorders (e.g., lupus), and certain blood clotting disorders can increase the risk.
-
Assisted Reproductive Technology: Pregnancies achieved through in vitro fertilization (IVF) or other assisted reproductive technologies may carry a higher risk of preeclampsia.
4. Diagnosis of Preeclampsia
Preeclampsia is diagnosed based on a combination of high blood pressure and the presence of other symptoms, such as proteinuria. Diagnostic criteria may include:
-
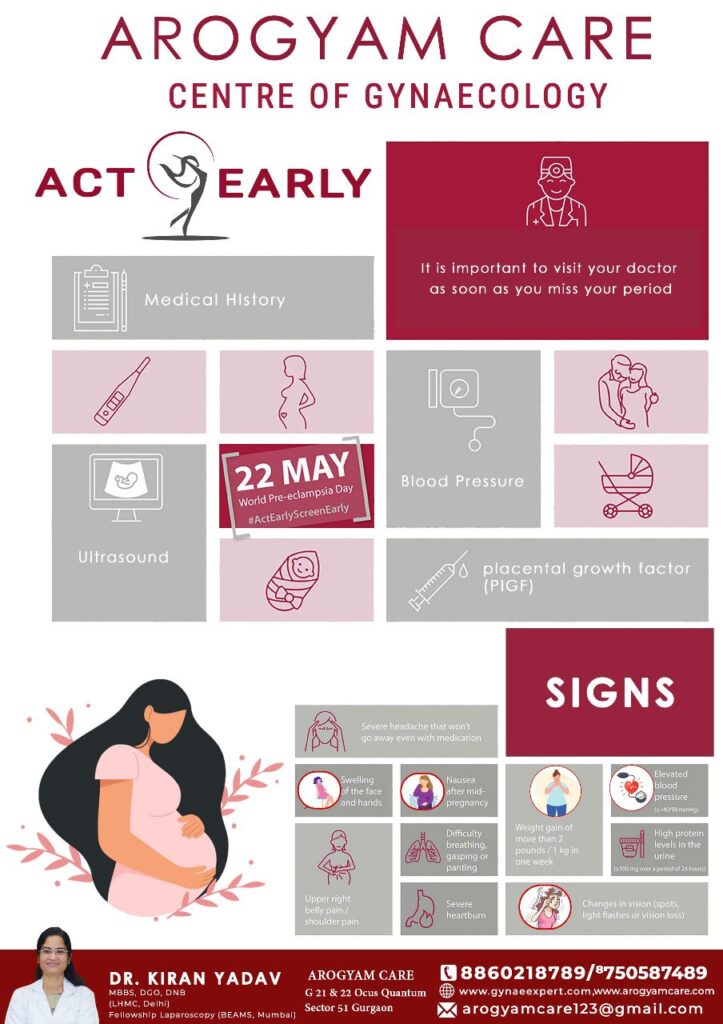
Blood Pressure Measurements: Blood pressure readings of 140/90 mm Hg or higher on two occasions, at least four hours apart, after 20 weeks of pregnancy, indicate hypertension associated with preeclampsia.
-
Urine Tests: A urine test showing proteinuria, typically more than 300 milligrams of protein in a 24-hour urine sample, supports the diagnosis.
-
Blood Tests: Blood tests can help assess kidney and liver function, as well as platelet count, to evaluate the severity of preeclampsia.
-
Fetal Monitoring: Ultrasound and fetal heart rate monitoring may be conducted to assess the baby’s well-being and growth.
5. Complications of Preeclampsia
Preeclampsia can lead to serious complications for both the mother and the baby if left untreated or not managed properly:
-
Eclampsia: This is a severe complication of preeclampsia that involves seizures. Eclampsia can cause serious harm to both the mother and baby and is a medical emergency.
-
HELLP Syndrome: HELLP syndrome is a life-threatening liver disorder that can occur in conjunction with preeclampsia. It stands for Hemolysis (destruction of red blood cells), Elevated Liver enzymes, and Low Platelet count. Symptoms include severe headaches, nausea, vomiting, upper right abdominal pain, and jaundice.
-
Organ Damage: Preeclampsia can affect the liver, kidneys, heart, and lungs, leading to organ damage and failure.
-
Placental Abruption: The placenta can detach from the uterus prematurely, causing heavy bleeding and posing a risk to both the mother and baby.
-
Preterm Birth: To protect the health of the mother and baby, early delivery may be necessary, leading to preterm birth and associated complications for the baby.
-
Intrauterine Growth Restriction (IUGR): Reduced blood flow to the placenta can result in poor fetal growth and low birth weight.
-
Maternal Mortality: In severe cases, untreated preeclampsia can lead to maternal death.
6. Treatment and Management of Preeclampsia
The primary treatment for preeclampsia is delivery of the baby, as the condition will typically resolve after birth. However, the timing of delivery depends on the severity of preeclampsia and the gestational age of the baby.
-
Mild Preeclampsia: If preeclampsia is mild and the pregnancy is less than 37 weeks, the healthcare provider may recommend bed rest, frequent monitoring, and medication to manage blood pressure. Corticosteroids may be administered to help accelerate the baby’s lung development in case early delivery becomes necessary.
-
Severe Preeclampsia: If preeclampsia is severe or the pregnancy is close to term (37 weeks or more), delivery is often the best course of action to protect both mother and baby. Hospitalization may be required to monitor the mother’s condition and manage symptoms. Magnesium sulfate may be administered to prevent seizures.
-
Blood Pressure Management: Medications to lower blood pressure, such as labetalol or nifedipine, may be prescribed to control hypertension and reduce the risk of complications.
-
Seizure Prevention: In cases of severe preeclampsia or eclampsia, magnesium sulfate is commonly used to prevent seizures.
7. Preventing Preeclampsia
While there is no guaranteed way to prevent preeclampsia, certain measures may help reduce the risk:
-
Regular Prenatal Care: Regular check-ups allow for early detection and management of high blood pressure and other risk factors.
-
Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain overall health and potentially reduce the risk of preeclampsia.
-
Regular Exercise: Engaging in regular physical activity can help manage weight, reduce blood pressure, and improve overall cardiovascular health.
-
Avoiding Smoking and Alcohol: Smoking and alcohol consumption can increase the risk of pregnancy complications, including preeclampsia.
-
Managing Chronic Conditions: Proper management of chronic conditions like hypertension, diabetes, and kidney disease can reduce the risk of preeclampsia.
-
Aspirin Therapy: Low-dose aspirin (81 mg daily) may be recommended for women at high risk of preeclampsia, starting in the second trimester, under the guidance of a healthcare provider.
Risk Factors:
- Primigravida,
- multifetal gestation- twins, triplets
- family history of pre-eclampsia ,
- h/o raised BP in previous pregnancy
- Obesity
Warning Signs:
- Headache
- blurring of vision
- epigastric pain
- nausea
- vomiting
- dizziness
- excessive swelling over feet and abdomen
- shortness of breadth
Conclusion
Preeclampsia is a serious pregnancy complication that requires careful monitoring and management to ensure the health and safety of both the mother and baby. By understanding the signs, risk factors, and treatment options for preeclampsia, expectant mothers can take proactive steps to reduce their risk and seek timely medical care. Early detection, regular prenatal care, and close monitoring by healthcare providers are essential for managing preeclampsia and ensuring a positive outcome for both mother and child.




I was reading some of your posts on this site and I believe this
internet site is real informative! Keep on putting up.
Real Estate I do not even understand how I ended up here, but I assumed this publish used to be great