Understanding Septal Resection: Procedures, Benefits, and Outcomes
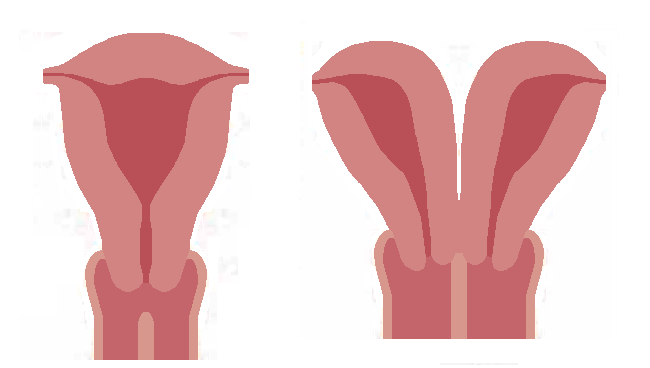
A septate uterus is a congenital condition where the two ducts that form your uterus do not fuse properly resulting in a wall of tissue (called the septum) that divides uterus into two parts. The septum can vary in length and thickness, and it can extend from the top of your uterus to cervix or even vagina. A septate uterus occurs in about 4% of people. The septum can interfere with the implantation of the fertilized egg, reduce the blood supply to the developing embryo, or cause abnormal contractions of the uterine muscles. These factors can increase the risk of infertility, miscarriage, preterm labor, fetal growth restriction, malpresentation, placental abruption, and cesarean delivery.
What is Septal Resection?
Septal resection is a surgical procedure primarily performed to remove a portion of the nasal septum or the heart’s septum. Depending on the context, the term may refer to different procedures in either otolaryngology (ear, nose, and throat) or cardiology. This overview will address both applications, focusing on their purposes, techniques, and outcomes.
1. Septal Resection in Otolaryngology
In the context of otolaryngology, septal resection involves the surgical removal of a portion of the nasal septum, which is the cartilage and bone that separates the two nostrils. This procedure is often indicated for patients with:
-
Severe Deviated Septum: A significant deviation can obstruct airflow, leading to breathing difficulties, chronic sinusitis, and sleep apnea.
-
Nasal Obstruction: Patients may experience persistent nasal congestion that doesn’t respond to medical treatments.
-
Nasal Polyps or Tumors: In some cases, the presence of polyps or benign tumors may necessitate resection for proper diagnosis and treatment.
A. Procedure Overview
-
Preoperative Assessment: Patients undergo a thorough evaluation, including imaging studies (like CT scans) and a physical examination.
-
Anesthesia: The procedure is typically performed under local or general anesthesia.
-
Surgical Technique: The surgeon makes incisions in the nasal lining to access the septum. Portions of the deviated septum, along with any obstructive tissue, are then removed. The remaining septal structure is often reshaped to improve airflow.
-
Recovery: Patients may experience swelling, bruising, and nasal congestion post-surgery. Recovery time varies, but many individuals return to normal activities within a week.
2. Septal Resection in Cardiology
In cardiology, septal resection refers to the surgical removal of a portion of the heart’s septum, usually the interventricular septum, which separates the left and right ventricles. This procedure is commonly performed in patients with:
-
Hypertrophic Cardiomyopathy (HCM): A condition characterized by abnormal thickening of the heart muscle, which can obstruct blood flow and lead to heart failure.
-
Obstructive Septal Hypertrophy: When the thickened septum obstructs blood flow from the heart to the aorta, leading to symptoms like chest pain, shortness of breath, and syncope.
A. Procedure Overview
-
Preoperative Assessment: Patients undergo comprehensive evaluations, including echocardiograms and other cardiac imaging techniques.
-
Anesthesia: The procedure is typically performed under general anesthesia.
-
Surgical Technique: Surgeons access the heart through a sternotomy (chest incision) or a minimally invasive approach. A portion of the thickened septum is resected to alleviate the obstruction, improving blood flow from the heart.
-
Recovery: Postoperative recovery may involve a hospital stay of several days, with ongoing monitoring. Most patients can gradually return to normal activities within a few weeks.
3. Risks and Considerations
While septal resection can provide significant benefits, there are risks associated with both procedures:
-
Nasal Septal Resection Risks:
- Infection
- Bleeding
- Changes in nasal shape or function
- Persistent nasal obstruction or discomfort
-
Cardiac Septal Resection Risks:
- Infection or bleeding
- Arrhythmias (irregular heartbeats)
- Heart failure or other complications
- Requirement for further surgeries
4. Outcomes and Benefits
Both types of septal resection can lead to substantial improvements in quality of life:
-
In Otolaryngology: Patients often experience enhanced breathing, reduced sinus infections, and improved overall nasal function.
-
In Cardiology: The procedure can alleviate symptoms of obstructive hypertrophic cardiomyopathy, improve exercise tolerance, and enhance overall cardiac function.
5. Conclusion
Septal resection, whether performed in the context of otolaryngology or cardiology, plays a vital role in treating conditions that significantly impact patients’ quality of life. With advances in surgical techniques and technology, these procedures can offer effective solutions, providing patients with improved health outcomes and enhanced well-being. As with any surgical intervention, thorough discussions with healthcare providers regarding risks, benefits, and expectations are essential for optimal results.

