Gynecological Surgery: Types, Indications, and Recovery
Gynecological surgery encompasses a wide range of procedures related to the female reproductive system, including the uterus, ovaries, fallopian tubes, cervix, and vagina. These surgeries are performed for various reasons, such as treating medical conditions, relieving symptoms, or addressing fertility issues. Depending on the procedure and the patient’s condition, gynecological surgery can range from minimally invasive techniques to more complex open surgeries.
1. Common Types of Gynecological Surgery
There are many types of gynecological surgeries, each tailored to specific conditions or health needs. Below are some of the most common procedures:
A. Hysterectomy
A hysterectomy involves the removal of the uterus and may be recommended for conditions such as uterine fibroids, endometriosis, abnormal bleeding, or cancer. There are different types of hysterectomies:
- Total Hysterectomy: Removal of the entire uterus, including the cervix.
- Partial (Subtotal) Hysterectomy: Only the upper part of the uterus is removed, leaving the cervix intact.
- Radical Hysterectomy: Typically performed for cancer, this procedure involves removing the uterus, cervix, and parts of surrounding tissues.
B. Laparoscopic Surgery
Laparoscopy is a minimally invasive surgery performed through small incisions in the abdomen. A camera is inserted to allow the surgeon to see inside the pelvic area. Common laparoscopic procedures include:
- Laparoscopic Hysterectomy
- Laparoscopic Ovarian Cystectomy (removal of ovarian cysts)
- Laparoscopic Tubal Ligation (for permanent birth control)
- Laparoscopic Endometriosis Treatment
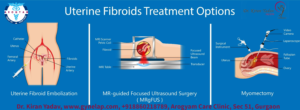
C. Myomectomy
A myomectomy is performed to remove uterine fibroids while preserving the uterus. This surgery is an option for women who wish to retain their fertility.
D. Ovarian Cystectomy
This procedure involves removing ovarian cysts that are causing pain, discomfort, or fertility issues. It may be performed through laparoscopy or open surgery, depending on the size and nature of the cyst.
E. Endometrial Ablation
Endometrial ablation is a minimally invasive procedure used to treat heavy menstrual bleeding by removing or destroying the lining of the uterus (endometrium). This procedure is often considered for women who have completed childbearing.
F. Colposcopy and LEEP
A colposcopy is a diagnostic procedure that examines the cervix for abnormal cells, often following an abnormal Pap smear. If abnormal tissue is found, a loop electrosurgical excision procedure (LEEP) may be performed to remove precancerous cells.
G. Pelvic Organ Prolapse Surgery
Pelvic organ prolapse occurs when the muscles and tissues supporting the pelvic organs weaken, causing the bladder, uterus, or rectum to descend into or out of the vaginal canal. Surgical procedures, such as vaginal or abdominal repairs, may be needed to correct this condition.
2. Indications for Gynecological Surgery
Gynecological surgery may be recommended for various medical conditions or health concerns. Some of the key indications include:
- Uterine Fibroids: Non-cancerous growths in the uterus can cause heavy bleeding, pain, or fertility issues. Myomectomy or hysterectomy may be needed.
- Endometriosis: This condition occurs when the tissue that normally lines the uterus grows outside it, causing pain and other symptoms. Laparoscopic surgery is often used to remove endometrial tissue.
- Ovarian Cysts: Large or persistent cysts on the ovaries may need to be surgically removed to prevent complications.
- Abnormal Uterine Bleeding: For women with heavy or irregular periods, surgery such as endometrial ablation or hysterectomy may be necessary.
- Gynecological Cancers: Cancers of the uterus, ovaries, cervix, or vagina may require surgical intervention, including hysterectomy, oophorectomy (removal of the ovaries), or debulking procedures.
- Pelvic Inflammatory Disease (PID): Severe infections that cause damage to reproductive organs may require surgery, especially if abscesses form.
- Ectopic Pregnancy: When a fertilized egg implants outside the uterus, usually in the fallopian tube, surgery is often required to prevent complications.
- Fertility Treatment: Surgical procedures like tubal ligation reversal or fibroid removal may be necessary for women seeking to improve fertility.
3. Minimally Invasive vs. Open Surgery
Many gynecological surgeries can now be performed using minimally invasive techniques, which offer numerous advantages over traditional open surgery, including:
- Smaller Incisions
- Less Scarring
- Reduced Pain and Recovery Time
- Lower Risk of Infection
- Shorter Hospital Stays
Minimally invasive surgeries, such as laparoscopy or robotic surgery, involve smaller incisions and the use of specialized instruments. In contrast, open surgery involves larger incisions and is usually reserved for more complex cases, such as certain types of cancer surgeries.
4. Preparing for Gynecological Surgery
Preparation for gynecological surgery depends on the type of procedure and individual health factors. Generally, patients should follow these steps:
- Pre-Surgical Evaluation: Patients may need to undergo blood tests, imaging studies, or other evaluations before surgery.
- Fasting: Most surgeries require fasting for a certain period before the procedure.
- Medications: Patients should inform their doctor about any medications they are taking. Some medications, especially blood thinners, may need to be stopped before surgery.
- Arrangements for Recovery: It’s essential to arrange for someone to drive the patient home after surgery and assist with daily activities during the initial recovery period.
5. Recovery After Gynecological Surgery
Recovery varies depending on the type of surgery performed. Minimally invasive procedures typically have shorter recovery times compared to open surgeries.
- Pain Management: Pain is common after surgery and can be managed with prescribed pain medications. Over-the-counter medications may also be recommended for less severe discomfort.
- Activity Restrictions: Patients are usually advised to avoid strenuous activity, heavy lifting, and sexual intercourse for a few weeks after surgery. Full recovery may take anywhere from a few days to several weeks, depending on the procedure.
- Follow-Up Care: Regular follow-up appointments are crucial to monitor healing, remove stitches if needed, and address any complications.
6. Potential Risks and Complications
As with any surgical procedure, gynecological surgeries carry some risks, including:
- Infection
- Bleeding
- Blood Clots
- Damage to Surrounding Organs
- Adverse Reactions to Anesthesia
- Scar Tissue Formation
Complications are rare, especially with minimally invasive surgeries, but it’s important to be aware of these risks and discuss them with the surgeon.
7. Emotional and Psychological Considerations
Gynecological surgery, particularly procedures like hysterectomy or surgeries related to fertility, can have emotional and psychological impacts. Women may experience feelings of loss, grief, or anxiety related to their reproductive health or changes in their body. Counseling or support groups can provide valuable emotional support during the recovery process.
Conclusion
Gynecological surgery plays a crucial role in treating a variety of conditions affecting women’s reproductive health. From minimally invasive procedures to more extensive surgeries, these interventions can improve quality of life, alleviate symptoms, and even prevent cancer. As surgical techniques continue to advance, many women can benefit from faster recovery times and fewer complications. It’s important to consult with a healthcare provider to understand the options, risks, and benefits tailored to individual health needs.




Very interesting details you have observed, thanks for putting
up.
Real Estate Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post .