Pregnancy is a journey filled with excitement and anticipation, but for some women, it comes with unique challenges. One such challenge is cervical insufficiency, a condition where the cervix begins to open prematurely, leading to a risk of preterm birth or miscarriage. A cervical stitch, also known as a cervical cerclage, can be a crucial intervention for this high-risk pregnancy.
What is Cervical Stitch?
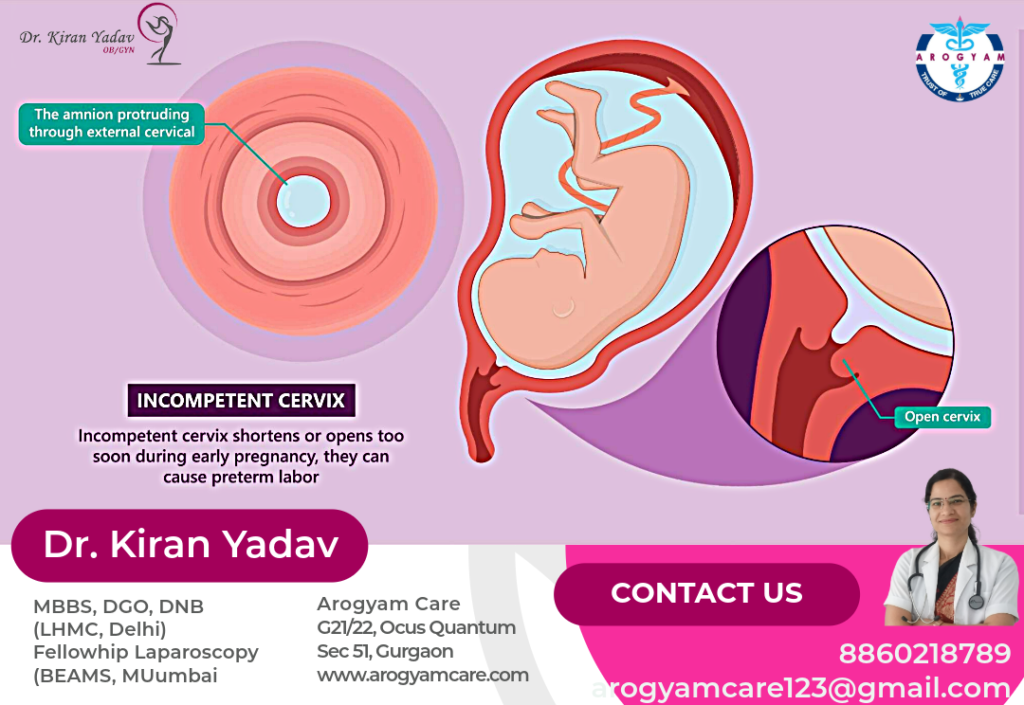
A cervical stitch, medically referred to as a cervical cerclage, is a procedure commonly used to address cervical insufficiency, a condition where the cervix begins to dilate (open) prematurely during pregnancy, often without pain or contractions. This early opening of the cervix can lead to a higher risk of preterm birth or miscarriage, particularly in the second trimester.
Why Is a Cervical Stitch Performed?
Cervical insufficiency can result from a variety of factors, including:
- Previous cervical surgery: Procedures like cone biopsy or treatments for cervical dysplasia can weaken the cervix.
- Congenital conditions: Some women are born with a naturally weak or short cervix.
- Trauma to the cervix: Injuries from previous childbirths or abortions may compromise cervical strength.
- Multiple pregnancies: Carrying multiple babies (twins, triplets, etc.) can put extra pressure on the cervix, increasing the risk of it opening prematurely.
Indications for Cervical Cerclage:
A cervical stitch is considered when:
- Cervical length is less than 25 mm: A short cervix identified through an ultrasound, particularly if there is a history of preterm birth or second-trimester miscarriage.
- History of preterm labor: Women who have previously had a preterm birth due to cervical insufficiency may benefit from a cerclage in subsequent pregnancies.
- Emergency cerclage: In cases where the cervix is found to be opening too early during pregnancy, an emergency cerclage might be placed even after the cervix has started to dilate.
Types of Cervical Cerclage:
- Prophylactic Cerclage: This preventive cerclage is usually performed between 12 and 14 weeks of pregnancy in women known to be at high risk of cervical insufficiency.
- Therapeutic Cerclage: This is done when an ultrasound shows early signs of cervical shortening but before any significant dilation has occurred, typically between 14 and 24 weeks.
- Emergency Cerclage (Rescue Cerclage): Performed when the cervix has already begun to dilate (with or without membranes protruding), often between 16 and 24 weeks of pregnancy.
The Procedure:
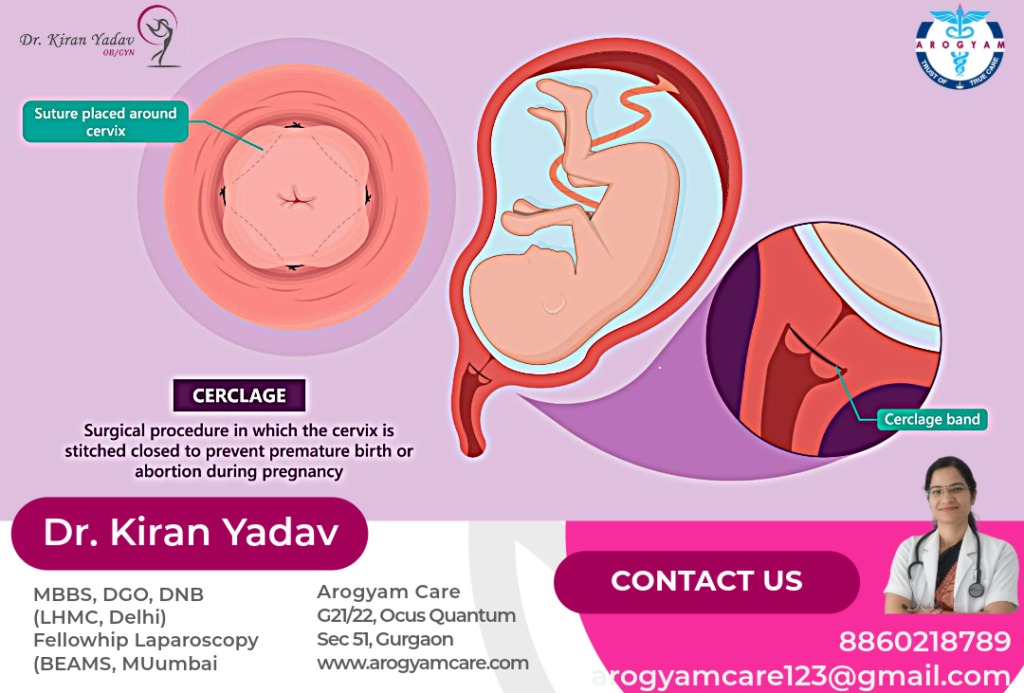
During the cerclage procedure:
1. Preparation: The patient is typically given regional anesthesia (like spinal or epidural anesthesia) to numb the lower half of the body, although general anesthesia may be used in some cases.
2. Placing the Stitch: The surgeon places a strong suture (stitch) around the cervix to hold it closed. This can be done vaginally (most common) or abdominally, depending on the situation.
3. Post-Procedure Care: After the stitch is placed, the patient may need to rest for a short period and will be monitored for signs of infection, preterm labor, or other complications. Sexual activity and strenuous exercise are typically restricted for some time following the procedure.
Removal of the Cervical Stitch:
- Timing: The stitch is usually removed around 37 weeks of pregnancy, or earlier if labor begins or if there are signs of complications, such as preterm contractions, bleeding, or infection.
- Process: Removal is typically a straightforward procedure done in an outpatient setting and usually does not require anesthesia.
Potential Risks and Complications:
While cervical cerclage is generally safe, there are some risks, including:
- Preterm labor: The procedure itself might trigger contractions in some women.
- Infection: There is a risk of infection, which can lead to preterm birth.
- Cervical damage: Rarely, placing or removing the stitch can cause injury to the cervix.
- Premature Rupture of Membranes (PROM): There is a small risk that the stitch could cause the membranes surrounding the baby to rupture prematurely, leading to complications.
Success and Efficacy:
Cervical cerclage is a widely used and effective procedure that significantly reduces the risk of preterm birth and miscarriage in women with cervical insufficiency. Success rates vary depending on the timing of the cerclage and the underlying condition of the cervix, but many women go on to deliver healthy, full-term babies after having a cerclage.
When is a cervical stitch needed?
Cervical cerclage is typically recommended for women who have:
- A history of second-trimester miscarriages due to cervical insufficiency.
- A short cervix identified through ultrasound during pregnancy.
- Previous cervical surgery that has weakened the cervix.
Types of Cervical Cerclage
There are three main types of cervical cerclage:
- Transvaginal Cerclage: The most common type, performed through the vagina.
- Transabdominal Cerclage: Performed through an abdominal incision, usually when a transvaginal cerclage has failed or is not possible.
- Emergency Cerclage: Performed when the cervix has already started to open.
The Procedure of Cervical Encerclage:
The procedure is usually done under regional anesthesia and involves the following steps:
- Preparation: The patient is positioned, and the cervix is cleaned.
- Stitch Placement: A strong suture is placed around the cervix and tied to keep it closed.
- Post-Procedure Care: The patient is monitored for a few hours before being discharged.
Post-Procedure Care
After the procedure, patients are advised to:
- Avoid heavy lifting and strenuous activities.
- Follow up regularly with their healthcare provider.
- Watch for signs of labor or infection.
Success Rates
Cervical cerclage has a high success rate, significantly reducing the risk of preterm birth in women with cervical insufficiency. However, the success largely depends on the timing of the procedure and the individual’s medical history.
Conclusion
A cervical stitch can be a vital intervention for women at risk of preterm birth due to cervical insufficiency. While it comes with its own set of risks, the benefits often outweigh them, offering hope and a safer path to full-term pregnancy.



Real Estate I appreciate you sharing this blog post. Thanks Again. Cool.